Otolaryngologist, head and neck surgeon Francis T. Hall discusses the evaluation of thyroid nodules, which primarily aims to determine the likelihood of malignancy. He then reviews the treatment of thyroid nodules and thyroid cancer, including recent advances in management
Fatty liver
Fatty liver
Fatty liver, once believed to be innocuous and of little importance, is becoming a significant liver disease that is increasing the global health burden. This article, written by Alan Fraser, discusses the prevalence, diagnosis and management of fatty liver. It concludes with a rapid guide to the interpretation of liver enzyme test results, including useful guidance for when more than one, or only one, liver enzyme is elevated
This How to Treat has been endorsed by the RNZCGP and has been approved for up to 1 credit for continuing professional development purposes (1 credit per learning hour). To claim your CPD credits, complete the assessment at the end of this page, then log in to your Te Whanake dashboard and record this activity under the appropriate learning category.
Nurses may also find that reading this article and reflecting on their learning can count as a professional development activity with the Nursing Council of New Zealand (up to 1 PD hour).
At the end of this course, you should be able to:
- Recognise the importance of fatty liver
- Discuss the diagnosis of fatty liver
- Describe treatment options for patients with fatty liver
- Interpret abnormal liver enzyme results
This How to Treat assists with the development of the following domains of competence in the general practice curriculum:
- Domain 1: Communication
- Domain 2: Clinical expertise
- Domain 3: Professionalism
- Domain 4: Scholarship
Fatty liver is the accumulation of lipid within hepatocytes and is the most common cause of elevated liver enzymes. Some patients will have excess alcohol intake as the underlying cause of fatty liver, but the majority will have non-alcohol-related fatty liver.
Fatty liver, while a descriptive term, lacks clarity. Non-alcoholic fatty liver disease (NAFLD) is a better term, although more cumbersome. It embraces the disease spectrum:
- fatty liver without inflammation
- fatty liver with inflammation
- fatty liver with significant fibrosis and/or cirrhosis.
The term non-alcoholic steatohepatitis or NASH is in common usage but, strictly, this term should only be used for fatty infiltration of the liver with proven inflammation. Recently, a change to metabolic-associated fatty liver disease (MAFLD) has been proposed. This is better as a positive definition, rather than simply stating that alcohol is not a factor.
What causes fatty liver?
The pathophysiology of NAFLD is believed to involve two steps, as discussed below.
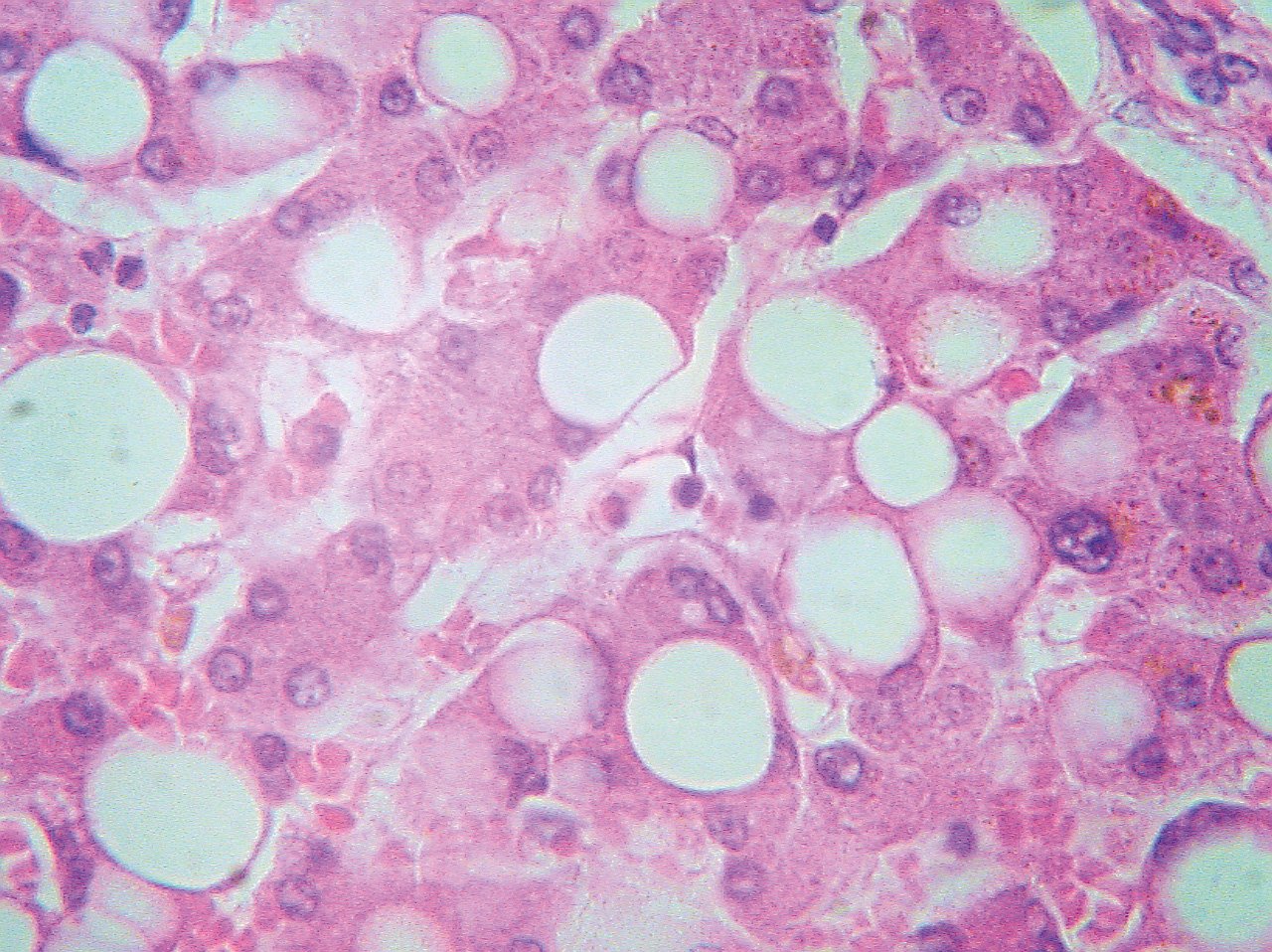
The first step is fat accumulation within hepatocytes (see Figure 1). The underlying problem is insulin resistance leading to an increase in peripheral lipolysis and a resultant increased delivery of free fatty acids to the liver. Normal metabolism requires free fatty acids to be “packaged” and secreted by the liver as very-low-density lipoprotein (VLDL). Triglycerides may accumulate in the liver, producing steatosis when the liver’s ability to make and secrete VLDL is exceeded. In a vicious cycle, steatosis may then promote further insulin resistance.
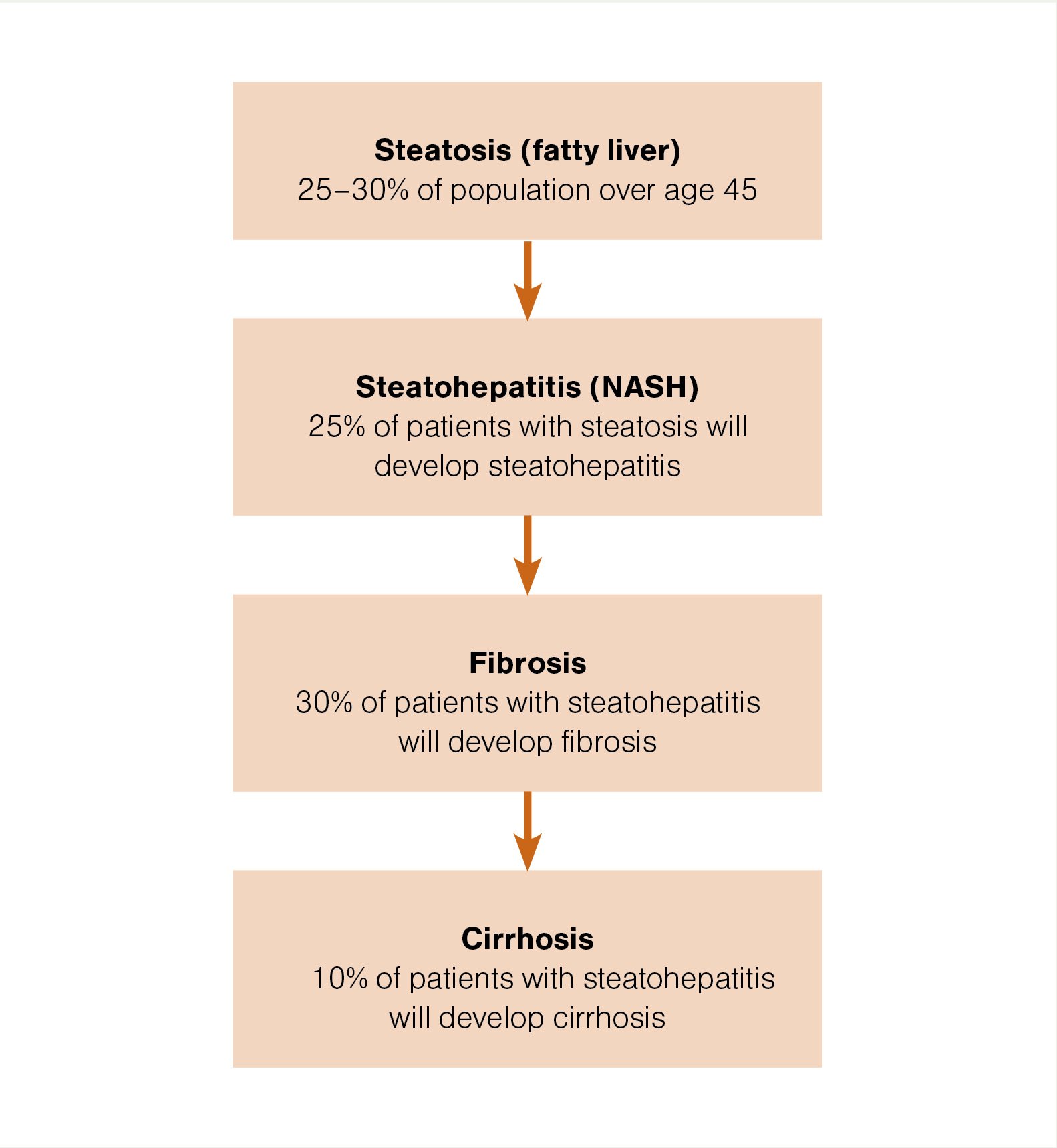
Approximately 25 per cent of patients with fatty accumulation will develop oxidative stress – the second step in the pathophysiology – which activates an inflammatory response (steatohepatitis). If sustained over a long period of time, this inflammatory process can lead to significant fibrosis and cirrhosis. At present, the mechanisms involved in the progression of steatosis to steatohepatitis are complex and not well understood.
NAFLD is an integral part of the metabolic syndrome and is therefore associated with obesity, increased waist circumference, hyperlipidaemia, type 2 diabetes, hypertension and hyperuricaemia. Fatty liver is a marker for significant insulin resistance and is associated with a twofold to fivefold risk of developing type 2 diabetes.
NAFLD is an independent risk factor for cardiovascular disease (ie, independent of age, gender, low-density lipoprotein cholesterol and smoking).
NAFLD is also associated with an increased risk of all-cause mortality. This is primarily from cardiovascular disease but also from liver-related deaths (cirrhosis and hepatocellular carcinoma), non-liver malignancy and complications of diabetes (including microvascular complications of retinopathy and renal disease).
NAFLD in pregnant women leads to a threefold increased risk of gestational diabetes and is associated with adverse maternal and perinatal outcomes.
The current worldwide prevalence of NAFLD, estimated by ultrasound imaging studies, is approaching 25 per cent and is likely to increase to 30 to 35 per cent by 2030. In New Zealand, prevalence is greater in Māori, Pacific and Indian populations, compared with the general population.
The majority of people affected have simple steatosis. It is more difficult to estimate the proportion with fatty liver who will have steatohepatitis, but a reasonable estimate is 25 per cent. The difficulty in estimation is because an accurate diagnosis requires liver biopsy, and most studies report on targeted biopsies of patients with higher clinical suspicion of steatohepatitis.
For patients with steatohepatitis, at least 25 to 30 per cent will develop significant fibrosis and 10 per cent will eventually develop cirrhosis (Figure 2).
In a large population-based study from the Netherlands, 33 per cent of individuals aged over 45 had evidence of NAFLD on ultrasound, and of those, clinically relevant fibrosis was detected by FibroScan in 8.4 per cent (17 per cent in individuals with diabetes).
The risk of cirrhosis increases with higher BMI and with type 2 diabetes – for example, 91 per cent of patients with obesity undergoing bariatric surgery have NAFLD. Most cases of cryptogenic cirrhosis (cause unknown) are actually due to steatohepatitis.
Importantly, there is an increasing prevalence of both obesity and type 2 diabetes worldwide and in New Zealand – this will impact on the number of patients with chronic liver disease from NAFLD.
Over the next 20 years, there will be a twofold to threefold increase in the number of patients with decompensated end-stage liver disease and a twofold increase in patients developing primary hepatocellular carcinoma. End-stage liver disease from NAFLD will probably become the most common reason for liver transplantation.
There is a concern that adolescents and young adults with a high BMI have a significant risk for advanced liver disease and hepatocellular carcinoma.
Diagnosis – risk factors, tests, imaging
A diagnosis of “fatty liver” is usually made as a result of investigation of abnormal liver function tests or may arise from an incidental finding at ultrasound performed for other reasons – for example, investigation of right upper quadrant discomfort.
Fatty liver does not cause symptoms. The liver is usually of normal size, but mild hepatomegaly may be present.
The definition of NAFLD requires an assessment of alcohol consumption. Many cases may be due to a combination of effects (eg, alcohol plus insulin resistance). The liver is likely more susceptible to the toxic effects of alcohol with increasing levels of obesity. Therefore, five to 10 units of alcohol per week could be significant if other risk factors for fatty liver are present.
One study showed the risk of moderate alcohol intake (two standard drinks per day; less than 20g pure alcohol) causing NAFLD is fivefold for non-obese men, 15-fold for overweight men and 35-fold for obese men. However, this interaction between moderate alcohol consumption and obesity was not seen for women.
The diagnosis of fatty liver also requires the exclusion of other causes of chronic hepatitis. The minimum required tests are hepatitis B surface antigen, hepatitis C antibodies, iron, total iron-binding capacity, serum ferritin, and autoantibodies (antinuclear antibody [ANA] and smooth muscle antibody [SMA]).
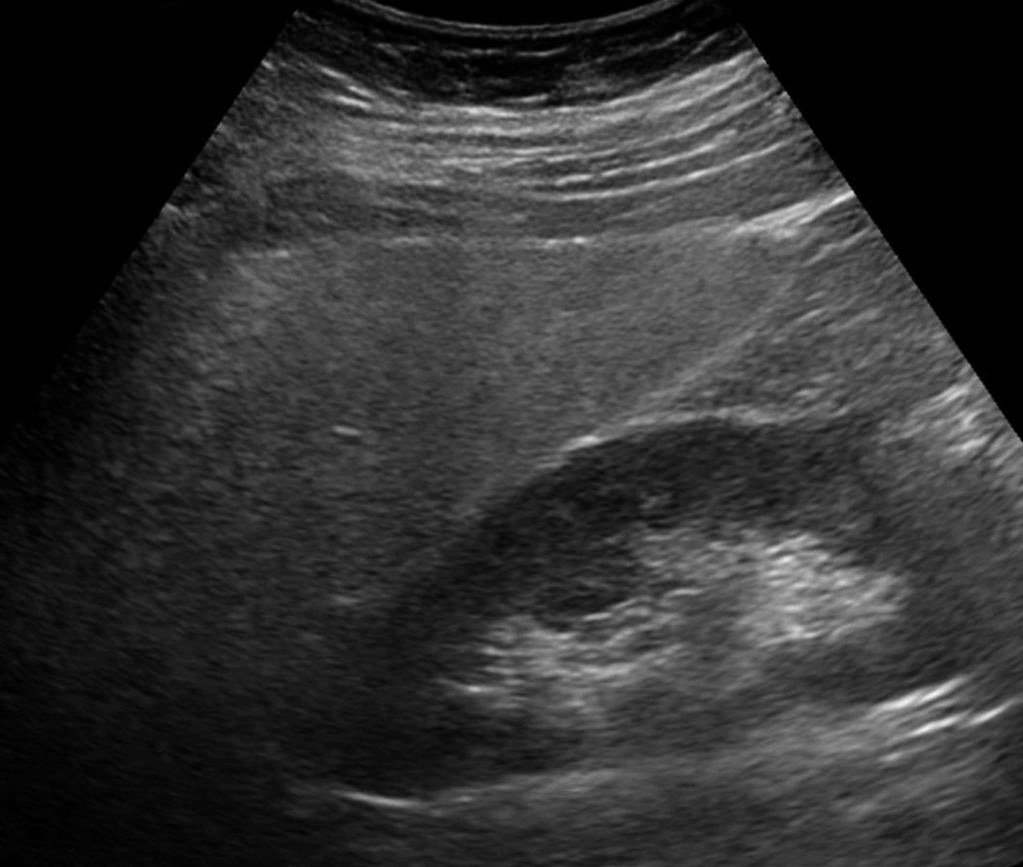
Ultrasound is reasonably sensitive for detecting fatty liver (sensitivity 70–85 per cent and specificity 80–90 per cent) and is a useful screening test (Figure 3). In the presence of risk factors for fatty liver, the diagnosis is still possible, indeed likely, even if the ultrasound is normal. Ultrasound cannot distinguish simple steatosis from steatohepatitis, and cirrhosis may be present with an ultrasound that simply shows fatty liver.
Abdominal CT scan is a potentially useful test, although accurate diagnosis depends on sensitive calibration of density scores. The distribution of fat in the liver is often “uneven” and can give the appearance of a focal lesion (focal fatty sparing).
Liver enzyme tests are helpful for determining steatohepatitis but are not reliable as the sole tool for assessment. The usual pattern seen is elevation of alanine aminotransferase (ALT) and gamma-glutamyl transferase (GGT). The level of ALT does not correlate well with steatohepatitis severity, but persistent elevation above 100IU/L definitely needs further evaluation. Significant steatohepatitis can occur with an ALT within the normal range.
Many predictive models and scoring systems for the risk of advanced steatohepatitis and fibrosis have been proposed but can be falsely reassuring. A Fibrosis-4 score >1.3 is considered intermediate to high risk for advanced fibrosis and should warrant referral (there are many FIB-4 calculators available online).
A FibroScan is a useful screening tool for fibrosis but has some limitation for the diagnosis of mild degrees of fibrosis, and obesity can prevent accurate assessment. Combining the FibroScan scores (the controlled attenuated parameter [CAP] gives an estimate of fat content, and the liver stiffness measurement [LSM] provides an estimate of fibrosis) with the aspartate aminotransferase (AST) level gives the FAST score, which has promise as a reliable marker for fibrosis. FibroScans are routinely available in secondary care, but primary care access may develop over time.
Metabolic syndrome and NAFLD
NAFLD should be suspected in patients with metabolic syndrome – central obesity, hyperlipidaemia (high triglycerides and low high-density lipoprotein cholesterol), type 2 diabetes (and prediabetes) and hypertension.
Waist circumference may be a better predictor for fatty liver than BMI; NAFLD can occur in patients with a normal BMI. Fasting lipid levels and HbA1c are an essential part of the investigation. A C-reactive protein level of 3mg/L or more without an obvious cause is also suggestive of significant fatty liver. An elevated serum ferritin level is common (due to hepatic inflammation, not iron accumulation).
Screening ultrasound for fatty liver is recommended for patients with type 2 diabetes and may be sensible when there are several features of metabolic syndrome present. Screening will become more valuable if treatment can be proven to reduce liver-related deaths.
Weight loss of 5 per cent in steatosis or 7 to 10 per cent in steatohepatitis is beneficial
An ideal treatment for fatty liver would treat the underlying insulin resistance, prevent the lipid peroxidation (and subsequent inflammatory process) and prevent hepatic fibrosis.
Weight loss, diet and exercise
Weight loss of 5 per cent in steatosis or 7 to 10 per cent in steatohepatitis is beneficial. The most intensive intervention trials report the highest losses in body weight and greater improvement in NAFLD.
The magnitude of improvement following exercise interventions appears to be less than with dietary interventions, and combination interventions seem to be most effective. Thus, the best strategy is a combination of moderate dietary restriction and 30 to 60 minutes of moderate-intensity exercise on three to five days each week.
Moderate-intensity activities include brisk walking, using a cross trainer, gardening or vigorous housework. These activities should induce a sustained increase in heart rate and an increased rate of breathing.
Weight loss using a very-low-calorie diet is typically greater than 10 per cent, but maintenance of weight loss is challenging in the long term. A low-carbohydrate diet may improve NAFLD more than other forms of dietary restriction; however, the evidence is mixed.
The Mediterranean-style diet (higher in monounsaturated fatty acids) has also been studied relative to a high-fat, low-carbohydrate diet for six weeks. No significant difference in weight loss resulted, but MRI results showed significant improvement in steatosis with the Mediterranean-style diet.
Exclusion of fructose may be important. Alcohol should be restricted to less than five units per week.
Medication
Metformin – clinical studies have not demonstrated a consistent benefit with metformin in patients with NAFLD, although this drug remains a good choice for patients with type 2 diabetes and obesity.
Vitamin E – fat-soluble vitamin E has antioxidant properties. Two large randomised controlled trials assessed its effect on adult and paediatric NAFLD populations. Treatment did meet the primary endpoint in both trials; however, there remains concern about long-term safety at the dose used (800IU per day), which appeared to increase all-cause mortality. Relapse occurred after stopping, suggesting this needs to be a long-term treatment.
Lipid-lowering drugs – statins and fibrates can be used to manage dyslipidaemia commonly found in patients with NAFLD. There are no studies to support a direct benefit of these drugs in NAFLD, but lipid lowering is important for reducing risk of cardiovascular events (along with antihypertensive medications). Patients with NAFLD do not have a higher risk for liver injury from statins.
Newer agents for type 2 diabetes – glucagon-like peptide-1 (GLP-1) receptor agonists have some useful effects beyond control of blood sugar and weight loss. Many randomised studies have confirmed reduction in steatohepatitis but no reduction in fibrosis (perhaps longer trials are required). There is enough evidence to suggest patients with type 2 diabetes and NAFLD should be on a GLP-1 receptor agonist. Funding restrictions prevent consideration of these drugs for patients without diabetes, but patients with obesity and NAFLD also benefit from GLP-1 receptor agonists.
Sodium-glucose cotransporter-2 (SGLT2) inhibitors reduce ALT levels and reduce liver fat, but the data are less convincing than for GLP-1 receptor agonists.
Bariatric surgery
Bariatric surgery improves or eliminates comorbid disease in most patients. There is improved long-term survival and reduced risk of death from cardiovascular disease and malignancy – the two most common causes of death in people with NAFLD.
A systematic review and meta-analysis of 32 studies of persons undergoing bariatric surgery, including 3093 liver biopsies obtained during and after bariatric surgery, reported that 66 per cent had complete resolution of steatosis, while 50 per cent and 76 per cent had resolution of inflammation and ballooning, respectively. Although fibrosis improved in 40 per cent of individuals, fibrosis worsened in approximately 12 per cent. Of note, the overall quality of the individual studies included was low.
The extent of weight loss is the main factor associated with decreased liver injury and not the type of surgery.
Summary
Fatty liver has emerged from a neglected condition, believed to be innocuous and of no importance, to being a significant liver disease that is increasing the global health burden.
The future task is to identify patients at risk of progression, preferably in a non-invasive way, and to provide effective treatments to these at-risk patients that can reduce overall mortality.
Presentation and history
Kane is a generally well, 28-year-old male non-smoker, whose alcohol intake is one to two units each week. Over the past four years, he has gradually gained weight, from 105kg to 137kg.
He has previously been diagnosed as having hepatitis B, and he now has abnormal liver function tests as part of routine blood tests. Further past history is an appendectomy when he was very young. He currently does not take any medication.
Examination and investigations
Kane’s general examination is normal, although he has a moderate degree of central obesity. His abdomen is soft and non-tender, and liver span is normal by percussion.
Blood tests show Kane is hepatitis B surface-antigen positive and hepatitis B e-antigen negative; his liver function tests report an ALT of 79IU/L and AST of 59IU/L, with other tests normal. His hepatitis B DNA level is very low at 1.53log10 copies/mL.
Kane undergoes an abdominal ultrasound that shows a marked diffuse increase in echogenicity consistent with fatty liver. A FibroScan is well within the normal range at 4.5kPa (95 per cent of healthy people without liver disease have a score of <7.0kPa). HbA1c is elevated at 46mmol/mol, consistent with impaired glucose tolerance.
Diagnosis and management
Kane is advised that the abnormal liver enzyme results are due to fatty liver. He has chronic hepatitis B, but this is inactive, and he could be considered a “healthy carrier”. Antiviral treatment is not needed.
After his diagnosis of fatty liver, he makes some dietary changes and loses weight. His liver function tests should be monitored on a 12-monthly basis, mainly to encourage him to continue with the beneficial lifestyle changes.
Presentation and history
Jake is a 63-year-old non-smoker who has an alcohol intake of between one and three units per week. His weight has been at a maximum of about 120kg at times. He regularly exercises during the winter as he still plays rugby for his local senior social team, although he is less active over summer.
Jake had his first review at age 41 because of abnormal liver function tests. At that time, his GGT was 160IU/L and ALT was 139IU/L, he weighed 114kg and his abdominal ultrasound was normal.
He continued to have mildly abnormal liver function tests: in 2020, GGT was 107IU/L and ALT was 29IU/L (his weight had reduced to 99kg); in 2021 and 2022, respectively, his GGT was 228IU/L and 141IU/L, and his ALT was 83IU/L and 54IU/L.
He was started on atorvastatin in 2020 because of a raised cholesterol level of 6.3mmol/L (triglycerides 2.3mmol/L), and his cholesterol and triglyceride levels have reduced to 3.3mmol/L and 1.3mmol/L, respectively. Jake is now uncertain if he wishes to continue with the statin because he wonders whether his abnormal liver function tests could be related to the medication.
Examination and investigations
Jake has a BMI of 30.7kg/m2 and moderate central obesity, with a waist measurement of 112cm. His abdomen is soft and non-tender. He has no signs of chronic liver disease, and his liver span is normal by percussion, with liver edge not palpable.
Jake undergoes an abdominal ultrasound, which shows mild increased echotexture consistent with mild fatty liver. Hepatitis C antibody is negative, hepatitis B antibody is <10mIU/mL, ferritin is 285μg/L and antinuclear antibody is negative.
Diagnosis and management
Jake’s diagnosis is NAFLD. His initial abdominal ultrasound was normal (30 per cent of cases will have normal ultrasound), and his ALT level has been mostly <100IU/L. When he is able to reduce his weight to 100kg, the ALT becomes normal.
He has had an excellent response to atorvastatin, with reduction in both total cholesterol and triglyceride levels, and he should continue with this medication. Jake needs to continue to lose weight – even a 5kg weight loss would be of major benefit. He also requires more regular aerobic exercise – three times a week for up to an hour each time.
Details of case studies have been changed to protect patient confidentiality
Liver enzyme tests can provide valuable assistance in evaluating hepatic dysfunction. However, the interpretation of abnormal liver enzyme results can often be challenging, and not everyone who has one or more abnormalities in these tests actually has liver disease.
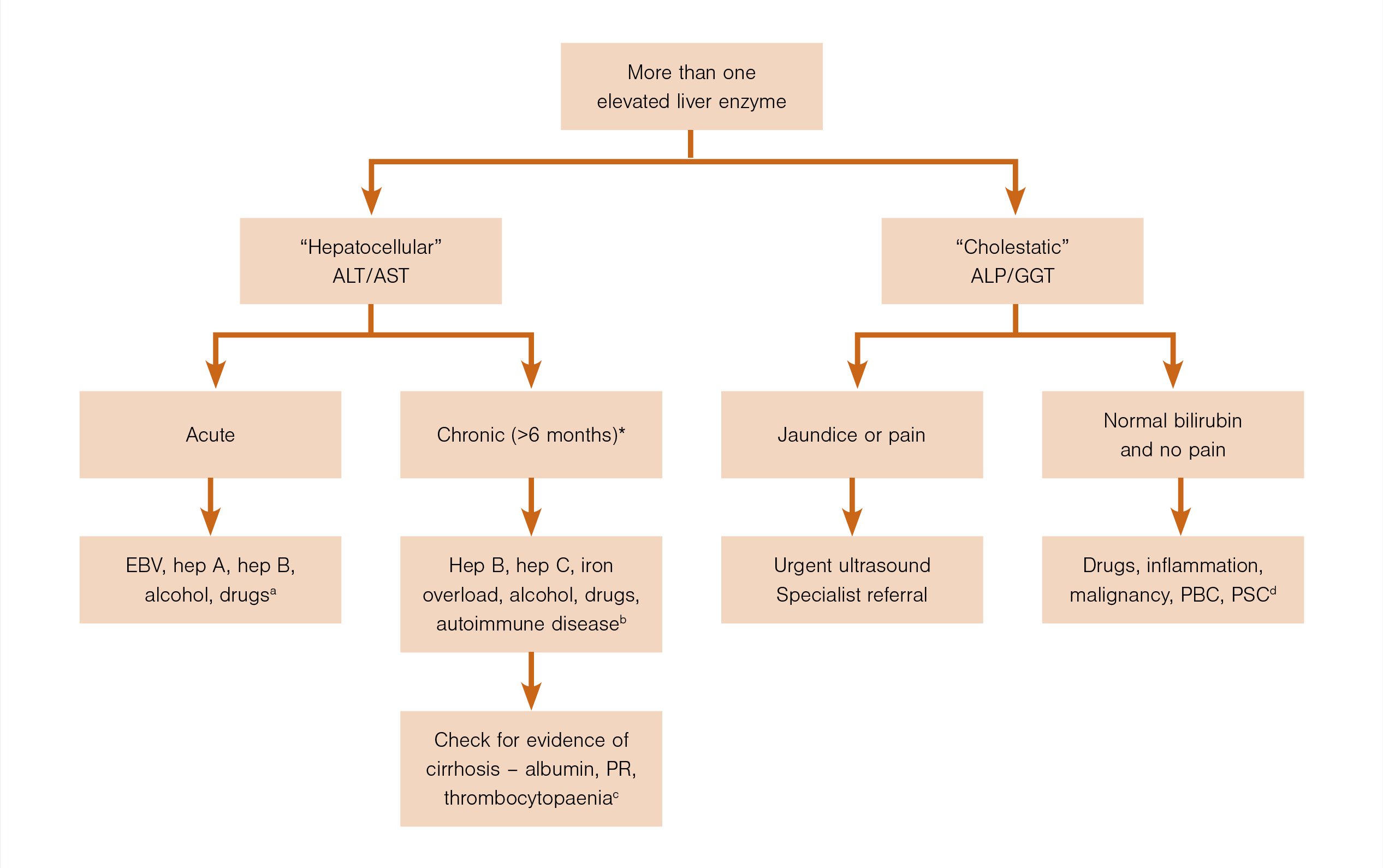
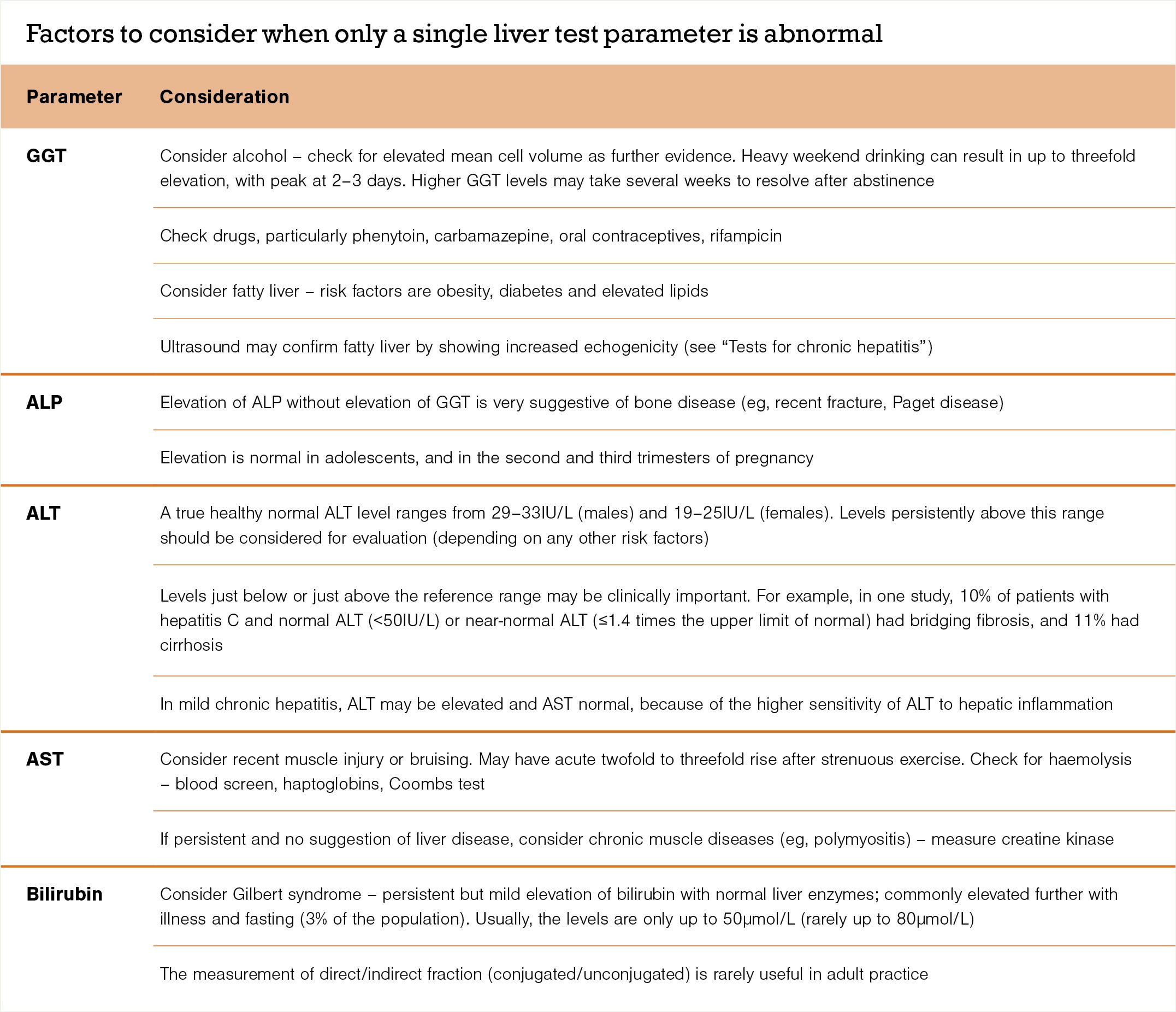
This guide intends to provide easily accessible information for GPs on appropriate investigations and likely diagnoses. The laboratory may report elevations in several liver enzymes (Figure 4) or in only a single enzyme or parameter (see table).
A full evaluation of liver function will always depend on careful history, examination and appropriate investigations.
Figure 4. Algorithm for guidance when more than one liver enzyme test is elevated
ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; EBV, Epstein–Barr virus; GGT, gamma-glutamyl transferase; hep, hepatitis; PBC, primary biliary cholangitis; PR, prothrombin ratio; PSC, primary sclerosing cholangitis.
* >6 months is the strict definition, but testing for potential causes should start after 1–2 months.
(a) See “Tests for acute hepatitis”; (b) see “Tests for chronic hepatitis”; (c) see “Check for evidence of cirrhosis”; (d) see “‘Cholestatic’ pattern, no pain or jaundice”
What to ask
When interpreting liver enzyme test results, common questions to ask are:
1. Is the pattern “hepatocellular” (mainly ALT/AST elevation) or is it “cholestatic” (mainly alkaline phosphatase [ALP] and GGT elevation)?
- If it is mainly hepatocellular, refer to question 2 below.
- If it is a mixture of both “patterns”, the predominant problem is usually obvious.
- In chronic hepatitis, mild cholestasis is common, but the pattern is predominantly hepatocellular.
- In acute biliary obstruction, ALT/AST levels may rise during the first two to three days (in addition to the cholestatic picture) but return to near normal if obstruction persists. Note that acute obstruction is usually associated with “biliary-type” pain.
- Biliary-type pain with cholestatic liver enzymes requires urgent specialist review even if an ultrasound is normal. The most likely cause is stones in the common bile duct. Magnetic resonance cholangiography may be required if there is diagnostic uncertainty.
- Reasons for a cholestatic pattern with no pain or jaundice are covered in a later section.
2. Is there evidence of persistent elevation of ALT/AST levels over more than one to two months?
- More than six months of elevated ALT/AST levels defines chronic hepatitis.
- In practical terms, chronic hepatitis should be considered from the onset and becomes more likely if there are persistent abnormalities after one to two months.
- Many patients with newly discovered elevation of ALT/AST will prove to have chronic liver disease.
- If the initial level of ALT/AST is greater than 500IU/L, it is most likely to be acute hepatitis/liver injury.
Tests for acute hepatitis
A diagnosis of alcohol-related liver disease rests primarily on the patient’s history and a high index of suspicion, rather than the pattern of liver enzyme test results
Acute hepatitis is usually associated with symptoms of an “acute illness”.
The main tests for acute viral hepatitis are hepatitis A immunoglobulin M and hepatitis B surface antigen, and tests for cytomegalovirus (<2 per cent of acute viral hepatitis cases) and Epstein–Barr virus (50 per cent) – the most common cause of acutely elevated ALT/AST levels in the community is infectious mononucleosis.
Hepatitis C does cause acute hepatitis but is almost always asymptomatic, and hepatitis D only occurs in the presence of hepatitis B infection.
Consider drugs as a cause of acute hepatitis. These can include phenytoin, isoniazid, diclofenac, allopurinol andazathioprine. Your patient may also have rash, fever and eosinophilia.
Also consider alcohol-induced liver disease. This may cause “hepatitis”, with AST and ALT levels that are relatively low for acute hepatitis (100–300IU/L). Look for elevated GGT (100–300IU/L) but normal ALP levels, macrocytosis, an AST level greater than ALT (a ratio >2.0 is very suggestive of alcohol-induced liver disease), elevated white blood cell count and fever if the hepatitis is more severe. A diagnosis of alcohol-related liver disease rests primarily on the patient’s history and a high index of suspicion, rather than the pattern of liver enzyme test results.
Rarely does autoimmune hepatitis present as an acute illness, and even rarer is Wilson disease. The latter can be considered if the patient is aged less than 40 – check serum copper and caeruloplasmin.
Paracetamol overdose will elevate the ALT level to over 1000IU/L. Check the INR. Most patients will need emergency department review.
Massive elevations in the ALT level are only seen in hospital settings and are predominantly due to cardiogenic shock and ischaemic hepatitis.
Acute hepatic vein obstruction can occur, particularly in the setting of haematological malignancy.
Tests for chronic hepatitis
In chronic hepatitis, the ALT level is usually only 1.5–3 times the upper limit of normal. If ALT levels have been elevated for more than one to two months, order the relevant tests – request hepatitis B surface antigen, hepatitis C antibodies (if positive, follow with hepatitis C PCR), autoantibodies (ANA and SMA), serum ferritin and iron studies (iron and total iron-binding capacity).
The most common cause of raised ALT/AST levels is fatty liver. This is usually combined with a mild elevation of GGT.
Raised serum ferritin may be due to haemochromatosis but also occurs with liver inflammation (it is common with fatty liver and excess alcohol consumption). Request liver ultrasound and evaluate risk factors for fatty liver. If iron saturation is high (>50 per cent) or ferritin is greater than 750μg/L, order a gene test for haemochromatosis (C282Y mutation in the HFE gene).
As in acute hepatitis, consider drugs. Any drug can be associated with chronic hepatitis – isoniazid, nitrofurantoin, ketoconazole, NSAIDs. Also consider illicit drugs, anabolic steroids and herbal treatments.
Autoimmune hepatitis is associated with raised serum globulins (often over two times the normal level); check autoantibodies (ANA and SMA).
Check the alpha-fetoprotein level (elevated in primary hepatocellular cancer), particularly if there is suspicion of cirrhosis.
The ratio of AST to ALT is often discussed with reference to a diagnosis of alcohol-related liver disease. An AST:ALT ratio of 2:1 is suggestive, but this is seen in only 50 per cent of cases. Clinical suspicion and careful questioning are more important.
Check for evidence of cirrhosis
Impairment of hepatic function or portal hypertension indicate cirrhosis. It is important to look for impairment in all patients with chronic hepatitis.
Check the serum albumin level and prothrombin ratio. Even borderline abnormal results are likely to be significant in the setting of chronic hepatitis. Albumin is a plasma protein exclusively synthesised by the liver with a circulating half-life of three weeks. A reduction in serum albumin usually indicates liver disease of more than three weeks’ duration, although any significant illness can decrease albumin levels because of cytokine effects.
Thrombocytopaenia suggests portal hypertension. An enlarged spleen may be detected by ultrasound.
‘Cholestatic’ pattern, no pain or jaundice
Ultrasound is the key test when elevated liver enzymes show a cholestatic pattern with no pain or jaundice.
Cholestasis may be a non-specific feature of disseminated cancer. Metastatic disease of the liver usually has a mixed pattern, with only mild elevation of ALP and GGT levels. It is usually confirmed by ultrasound. If bile ducts are dilated and there is no biliary-type pain, the cause is likely to be malignant bile duct obstruction.
If the ultrasound is normal, several reasons for a cholestatic pattern need to be reviewed:
- Consider drugs.
- Phenothiazines – your patient can continue these if there is mild cholestasis (two to three times normal values for ALP and GGT). Remember that prochlorperazine (Stemetil) may cause cholestasis.
- Amoxicillin + clavulanic acid (Augmentin) and flucloxacillin – may cause a progressive cholestasis with slow resolution over several months after the drug is discontinued.
- Erythromycin – may present with acute right upper quadrant pain.
- Non-specific cholestasis is common with sepsis and in chronic inflammatory conditions (eg, inflammatory bowel disease).
- Mild elevation (mixed pattern) is common with predominant right-sided heart failure related to hepatic congestion.
- If cholestasis is chronic (more than three to six months) and progressive, consider chronic liver disorders, such as primary biliary cirrhosis and sclerosing cholangitis, and HIV cholangiopathy. Order anti-mitochondrial antibody. Specialist referral is required for magnetic resonance cholangiopancreatography with or without liver biopsy.
Asymptomatic benign liver lesions (usually haemangiomas) are common and are not associated with liver enzyme abnormalities.
Drugs and monitoring of liver enzymes
A definite benefit from regular monitoring of liver enzyme tests is evident in only a few examples:
- Isoniazid – only a transient elevation in liver enzymes is usual, but isoniazid must stop if a progressive rise is evident. Fulminant hepatitis may occur – the risk is higher if the patient’s age is over 50.
- Methotrexate – early elevation of ALT/AST levels can occur in the first few months after initiation, but this may not be important. Progressive changes may suggest hepatic fibrosis and need for further evaluation with a FibroScan.
- Azathioprine – hepatitis may occur in the first few months after initiation and require cessation of drug; 6-mercaptopurine may be a useful alternative.
- Statins – mild elevations of ALT are common, particularly in the first few months after beginning treatment, and usually related to underlying fatty liver (there may be shifts in intrahepatic lipids during initial treatment).
Role of liver biopsy
When investigating abnormal liver enzyme tests, the majority of diagnoses are made by undertaking a patient history (with a careful review of drug history), physical examination and blood tests. A FibroScan can diagnose or exclude advanced liver disease. Only a few patients will require a liver biopsy.
General considerations
Always ask about medication – prescribed and over the counter. Common agents that may cause a rise in liver enzymes are antibiotics, antiepileptics, NSAIDs and herbal products.
Rare and surprising causes of raised liver function test results are coeliac disease and both hypothyroidism and hyperthyroidism. Abnormal liver function tests in late pregnancy are often important and may need urgent review.
Should the diagnosis remain unclear in the presence of abnormal liver function test results:
- discontinue hepatotoxic drugs
- discontinue alcohol
- assess again for fatty liver and risk factors.
Read more in “Liver function tests in primary care” on the BPACnz website (bpac.org.nz/2022/LFTs.aspx).
Androutsakos T, Nasiri-Ansari N, Bakasis AD, et al. SGLT-2 inhibitors in NAFLD: Expanding their role beyond diabetes and cardioprotection. Int J Mol Sci 2022;23(6):3107.
Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology clinical practice guideline for the diagnosis and management of nonalcoholic fatty liver disease in primary care and endocrinology clinical settings: Co-sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract 2022;28(5):528–62.
Kawaguchi T, Charlton M, Kawaguchi A, et al. Effects of Mediterranean diet in patients with nonalcoholic fatty liver disease: A systematic review, meta-analysis, and meta-regression analysis of randomized controlled trials. Semin Liver Dis 2021;41(3):225–34.
Lee Y, Doumouras AG, Yu J, et al. Complete resolution of nonalcoholic fatty liver disease after bariatric surgery: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2019;17(6):1040–60.
Patel Chavez C, Cusi K, Kadiyala S. The emerging role of glucagonlike peptide-1 receptor agonists for the management of NAFLD. J Clin Endocrinol Metab 2022;107(1):29–38.
Younossi ZM, Corey KE, Lim JK. AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: Expert review. Gastroenterology 2021;160(3):912–18.
Alan Fraser is a gastroenterologist with Auckland Gastroenterology and associate professor of medicine at the University of Auckland
This 10-question multiple-choice assessment is designed to demonstrate that the provided educational reading has been effective in allowing you to meet the learning objectives of this course. Write down your answers to these questions.
1. Which statement regarding non-alcoholic fatty liver disease is correct?
a. Cardiovascular disease is the major cause of mortality in people with NAFLD
b. In New Zealand, NAFLD is most common in European populations
c. Right upper quadrant pain is a common symptom of NAFLD
d. The liver is usually found to be enlarged in patients with NAFLD
e. The worldwide prevalence of NAFLD is now decreasing
2. What is a reasonable estimate of the proportion of people who will progress from simple steatosis to steatohepatitis?
a. 5 per cent
b. 10 per cent
c. 25 per cent
d. 35 per cent
3. Which TWO of the following statements regarding the use of ultrasound for diagnosis of NAFLD are correct?
a. A diagnosis of NAFLD is still possible with a normal abdominal ultrasound
b. Abdominal ultrasound is useful for distinguishing simple steatosis from steatohepatitis
c. An ultrasound that shows diffuse increased echogenicity of the liver is consistent with NAFLD
d. An ultrasound that shows only fatty liver excludes the diagnosis of cirrhosis
4. Which statement regarding weight loss in patients with NAFLD is correct?
a. A low-fat diet is the best dietary pattern for patients with NAFLD
b. Exercise interventions appear more beneficial than dietary interventions
c. Exercise interventions should induce a sustained increase in heart rate and breathing rate
d. Weight loss needs to be at least 10 per cent of body weight to achieve any benefit
5. Which TWO of the following statements regarding pharmacological treatment of NAFLD are correct?
a. Pharmacological treatment options remain disappointing and are not an option for most patients
b. Lipid-lowering drugs should be used to treat dyslipidaemia, if present
c. Metformin has demonstrated consistent benefits for patients with NAFLD
d. Patients with type 2 diabetes and NAFLD should be on a funded GLP-1 receptor agonist
6. In patients with NAFLD and obesity, which of the following can be improved by bariatric surgery?
a. Comorbid disease
b. Fibrosis
c. Long-term survival
d. Steatohepatitis
e. All of the above
7. Which of the following is most likely with initial ALT/AST levels >500IU/L?
a. Acute hepatitis
b. Cholestatic hepatitis
c. Chronic hepatitis
d. Fatty liver
8. In patients with elevated ALT/AST levels, when should testing for potential causes of chronic hepatitis be performed?
a. At the outset
b. After 1–2 months of persistent elevation
c. After 6 months of persistent elevation
d. When the AST:ALT ratio is >2
9. Which TWO of the following statements regarding ALT and AST levels are correct?
a. AST has a higher sensitivity to hepatic inflammation than ALT
b. The ALT level correlates well with steatohepatitis severity
c. The ALT level will be higher than AST if there is muscle injury or bruising
d. The AST level is often higher than ALT in alcohol-induced liver disease
e. The most common cause of persistent ALT/AST elevation is fatty liver
10. A patient presents with a “cholestatic” liver enzyme pattern and biliary-type pain. What is the most likely cause (and what should you do)?
a. A liver haemangioma
b. Drugs such as erythromycin
c. Inflammatory bowel disease
d. Malignant bile duct obstruction
e. Stones in the common bile duct
Write down your answers to these questions. Then, to check your answers and record your score, click here.
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions, which align with Te Whanake reflection requirements (answer three or more):
- What were the key learnings from this activity?
- How does what you learnt benefit you, or why do you appreciate the learning?
- If you apply your learning, what are the benefits or implications for others?
- Think of a situation where you could apply this learning. What would you do differently now?
- If an opportunity to apply this learning comes up in the future, what measures can be taken to ensure the learning is applied?
- Can you think of any different ways you could apply this learning?
- Are there any skills you need to develop to apply this learning effectively?






![New Zealand Doctor Rata Aotearoa editor Barbara Fountain, RNZCGP president elect and Tauranga-based specialist GP Luke Bradford, Ministry of Health clinical chief advisor rural health Helen MacGregor, and Health New Zealand Te Whatu Ora clinical director primary and community care Sarah Clarke [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/1.%20Barbara%20Fountain%2C%20Luke%20Bradford%2C%20Helen%20MacGregor%20and%20Sarah%20Clarke.jpg?itok=091NETXI)
![Ngāti Porou Oranga specialist GP Elina Pekansaari and Te Nikau Hospital specialist in general practice and rural hospital medicine David Short [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/2.%20Elina%20Pekansaari%20and%20David%20Short.jpg?itok=h5XfSBVM)
![Locum specialist GP Margriet Dijkstra and OmniHealth regional operations manager (southern) Patricia Morais-Ross [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/3.%20Margriet%20Dijkstra%20and%20Patricia%20Morais-Ross.jpg?itok=jkrtRfJC)
![Golden Bay dairy farmer and dairy industry health and safety doctoral student Deborah Rhodes, and Golden Bay Community Health specialist GP Rachael Cowie [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/4.%20Deborah%20Rhodes%20and%20Rachael%20Cowie.jpg?itok=oM0_GcJc)
![Hauora Taiwhenua clinical director rural health Jeremy Webber, Australian College of Rural and Remote Medicine president Rod Martin and Observa Care director of business operations Deborah Martin, the wife of Dr Martin [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/5.%20Jeremy%20Webber%2C%20Rod%20Martin%20and%20Deborah%20Martin%2C%20the%20wife%20of%20Dr%20Martin.jpg?itok=P_aGmX_H)
![Spark Health chief executive John Macaskill-Smith and client director Bryan Bunz [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/6.%20John%20Macaskill-Smith%20and%20Bryan%20Bunz.jpg?itok=5yJvVZ0I)
![Associate dean (rural) Kyle Eggleton, third-year medical student Roselle Winter, and second-year pharmacy student Alina Khanal, all from the University of Auckland [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/7.%20Kyle%20Eggleton%2C%20Roselle%20Winter%20and%20Alina%20Khanal.jpg?itok=RQLd3TEs)
![Health New Zealand Te Whatu Ora clinical editor and specialist in general practice and rural hospital medicine Anu Shinnamon, and Whakarongorau chief clinical officer Ruth Large [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/8.%20Anu%20Shinnamon%20and%20Ruth%20Large.jpg?itok=i5TMswY9)
![Te Kahu Hauora Practice specialist GP Jane Laver and Ngāti Kahungunu ki Tāmaki-nui-a-Rua chief operations manager Tania Chamberlain [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/9.%20Jane%20Laver%20and%20Tania%20Chamberlain.jpg?itok=jtMklaCZ)