For older people and frail people, the long-term benefit of medicines reduces and the potential for harm from adverse effects increases. When the benefit–risk balance changes in this way, medicine review and optimisation are important to simplify the therapeutic regimen, reduce inappropriate medicines and minimise risks. In this article, pharmacist prescriber Linda Bryant uses two case studies to illustrate important considerations during medicine reviews
Shots fired at GPEP programme labelled as ‘attention seeking’
Shots fired at GPEP programme labelled as ‘attention seeking’
Essentials
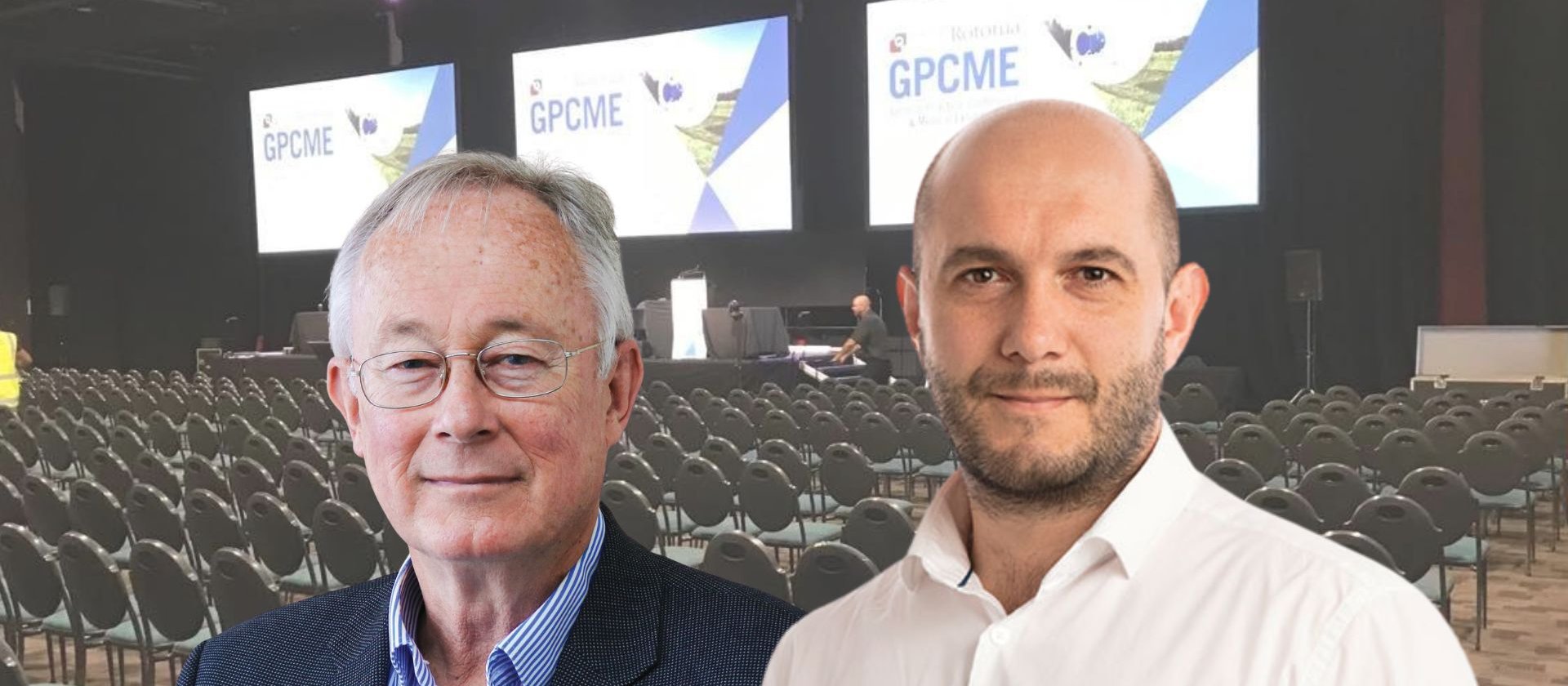
- Specialist GP and general practice professor Bruce Arroll slammed the current GPEP programme during a session exploring the merits of a third medical school at this year's Rotorua GPCME.
- Professor Arroll was arguing for a dedicated GP stream in medical school, provided by the two current universities.
- RNZCGP medical director Luke Bradford dismissed the claims as the “remarks of someone looking for attention”, saying GPEP graduates are “absolutely good GPs”.
Shots were fired at the GP training programme at the Rotorua GPCME, with a prominent general practice professor claiming it was “essentially a one-year programme”, and that hospital specialists were better trained.
Friday’s medicopolitical plenary session – ostensibly on the topic of a third medical school at Waikato University – saw a number of shots fired at the RNZCGP while medical director and president-elect Luke Bradford sat waiting for his turn to speak.
Bruce Arroll, a professor in general practice at the University of Auckland and a specialist GP at the Calder Clinic at the Auckland City Mission, presented an alternative to a third medical school – creating a GP stream in the current medical schools at Auckland and Otago universities.
“[GPEP] is essentially a one-year programme, so no wonder our hospital specialists are well trained”
His idea was based on the current model – of six years at medical school, two years as a house officer, and then a number of years training in a chosen discipline – being too hospital focused. “I think this has failed New Zealand general practice,” Professor Arroll told the conference session.
“I think our hospital doctors are extremely well-trained because they’ve had five or six years in training, our GPs are not – they become very good doctors over time – certainly not when they finish their GP training programme,” he said. “It’s essentially a one-year programme, so no wonder our hospital specialists are well trained…I think our GP trainees become good, although there’s no guarantee that they are.”
Professor Arroll’s idea consisted of a medical school GP stream in which students would sign up for at the beginning of medical school. Prospective GPs would complete three or four years of medical school and then one year of GPEP before qualifying as a GP. There would be no house surgeon years and ideally there would be a zero-fees policy for doctors who stayed in New Zealand for five of the 10 years following graduation.
“You’d be a really good family doctor if you had four years of training,” Professor Arroll said. “You could do all sorts of things – you could inject any part of the body, you’d know how to do a sleep consult, you could do a good mental health consult, the dermatology wouldn’t terrify you.
“You’d be really good, you’d be like the hospital docs where you could do everything within your discipline, and if you pass that you get your FRNZCGP. The regular people, who came through the regular stream, two-year house surgeons, would do the three years GPEP.”
Professor Arroll believed his idea would be popular with the public, but conceded there might be push-back on it being a “second-class degree”. However, he disputed that, saying: “Overseas people and Australia would be lapping up our graduates.”
He said: “Actually the problem might be you just might be too well trained. The surgical programme might quite like people who are really good at something.
“I mean, after eight years you still can’t do anything on your own. Just think about it – step back from what you know, and I say, ‘I’ve got a course and after eight years you can’t do anything, we still can’t let you loose without some sort of supervision’. That’s not a very efficient programme.”
Big-tech companies “would throw up their hands in horror” at such a situation, he said.
Dr Bradford, who made reference to some “accusations” when he took to the lectern, didn’t respond on stage, but speaking to New Zealand Doctor Rata Aotearoa branded the comments about the GPEP programme as an “off-the-cuff remark that was unjustifiable”.
“I think when people have done the three-year training and the assessments, then they are absolutely good GPs and we’re very proud to have them as specialist GPs,” he said. “Can we improve the support given in those two years [GPEP 2 and 3] and the resources and time allocated to those trainees to learn? Absolutely, and that is one of our priorities.”
The Tauranga-based specialist GP added: “What I thought was absurd was he, on one hand said we’ve got doctors leaving after three years of GP training who aren’t good enough to be GPs, and on the other hand said what we should do instead is train them for three years at university and give them one year as GPs and call them GPs.
“Well, that makes absolutely no sense to me at all – he wants to go from 11 years of learning, saying that’s not good enough, to four years which suddenly is? I mean, it’s just remarks of someone looking for attention.”
Asked if there was any merit in the idea of having a GP stream at medical school, Dr Bradford said: “No, absolutely, categorically not.”
The college is in favour of medical students having more exposure to general practice including the Government’s proposed PGY2 in general practice, he said. “But what was being proposed was an entirely two-tier [system]. The GPs on Bruce’s scheme would not be recognisable as doctors anywhere else in the world or amongst their colleagues and that is categorically against what we believe should be the case.”
He disputed Professor Arroll’s assertion that the GP graduates from his scheme would be sought after around the world, saying: “They wouldn’t be allowed to go anywhere in the rest of the world, because the rest of the world insists on them going through a proper medical degree.”
It was important for GPs to have experience in hospitals, partly for the collegiality, and also for the understanding of hospital medicine, which is “necessary if you’re going to spend the rest of your life interfacing with it, which is what we do”.
“Do I think we need to have a look at the whole 11-year training programme to graduate as a GP Fellow? Yes, I think the whole of medicine needs to look at itself for that. I think the public, and the politicians certainly, are running out of patience with how long it takes us to get there and so I think that is something that needs addressing.”
However, Dr Bradford didn’t think shortening the GPEP programme was the answer, favouring a reduction in medical school years in line with international programmes to about four or five years, instead of six. But he said it might be possible in future – pending curriculum and skills log assessment – to reduce GPEP if a trainee had spent a full year in general practice in the PGY2 run.







